7 Major Causes of Fungal Acne on Face

What Is Fungal Acne?
Fungal acne is a type of skin infection in the hair follicles of the skin. It usually appears as small pimples that don't vary much in shape or size, often with itching.
Fungal acne can cause skin irritation and whiteheads. It is often confused with acne vulgaris. It is the type of acne commonly associated with black and whiteheads.
But fungal acne and acne vulgaris are conditions caused by two other things. They will not respond to the same treatment. If you continue using anti-acne therapies, you can worsen fungal acne.
It’s essential to understand what fungal acne looks like and how it develops. Read on to learn the major causes and symptoms of fungal acne and what you can do to treat and prevent breakouts.
Fungal Acne Is Folliculitis

Folliculitis causes inflammation and infection of your hair follicle, causing pimples on the skin. You can get folliculitis in every part of you have hair.
Sometimes people think they have acne, but treatment doesn't improve. Usually, it is a sign that you don't have acne but a fungal infection in the hair follicle.
It is called Pterosporum folliculitis. It causes by Malassezia species and usually affects teenagers due to excess oil production in the skin. It is generally found on your back, shoulders, and neck and can be caused by sweating. It refers to a yeast infection.
Other Types of Folliculitis
The yeast infection is often confused with acne, But can also misdiagnose as superficial bacterial folliculitis. There are different kinds of folliculitis, including.
- Superficial bacterial folliculitis: It is a common type of folliculitis. It is caused by Staphylococcus aureus bacterial infection. Your skin typically contains these bacteria. If you damage the hair follicle, causing the follicle to become irritated, bacteria can enter the area and cause an infection.
- Viral folliculitis: The herpes virus can cause folliculitis. Viral folliculitis often looks bacterial but has clusters of spots and plaques. Molluscum contagiosum can sometimes cause viral folliculitis, but this is less common.
- Gram-negative bacterial folliculitis: It is also known as hot tub folliculitis, caused by Pseudomonas aeruginosa bacteria. It comes from contaminated water, poorly treated hot tubs, or a swimming pool. Klebsiella and Enterobacter species of bacteria can also cause this type of folliculitis. These usually occur after taking antibiotics for a long time.
- Demodex folliculitis: The Demodex folliculorum can causes this type of folliculitis. Most people's skin clears up without folliculitis developing, but some people with pre-existing skin conditions or weakened immune systems react differently.
- Eosinophilic folliculitis: If you have HIV, you may develop this type of folliculitis. It's unclear what causes this, but it may be a side effect of chemotherapy. It usually appears on the scalp, face, and neck and resembles a hive.
- Pseudofolliculitis Barbie: This type of folliculitis is also called razor bumps and doesn't always cause a skin infection. It usually happens to people with curly beards. After shaving, the hair melts back into the skin and grows, causing inflammation and bumps.
What Major Causes Fungal Acne?

Fungal acne is a misnomer. Unlike acne, fungal acne is not primarily caused by bacteria and oil in the pores. However, oil and sebum production is a big part of helping to feed the bacteria that cause fungal acne.
Instead, the rash-like rashes and irritated skin are associated with fungal acne caused by a type of yeast, a kind of fungus.
That is why sometimes it is called fungal acne. It is also called Malassezia folliculitis or Pityrosporum folliculitis.
The responsible yeast of fungal acne is present on the skin constantly. Usually, your body can balance the yeast, other fungi, and bacteria that are also part of your skin.
But if that natural balance is disturbed, it can become too much. It is when the hair follicles become infected, and symptoms such as acne appear.
What type of acne you are facing? These are most common types of acne. You must know about the type of acne, And know how to resolve it.
Several events or conditions can upset this balance of bacteria and fungi, including:
- Trapped moisture: Wearing sweaty workout clothes for long periods can promote yeast growth. Wearing workout clothes again without washing them can also expose your skin to the fungus that grows in the clothes.
- Treatment: If you take antibiotics, the bacteria on your skin may decrease.
- A suppressed immune system: People with weakened immune systems are more likely to develop fungal acne.
- Dietary changes: Fungi and yeast feed on carbohydrates, so balancing your intake of sweets and carbohydrate-rich foods can help slow fungal growth.
- Wear tight clothes: Regularly wearing non-breathable clothing can encourage excess sweat and moisture. It can promote a skin environment for yeast to grow.
- Warm, humid environment: People living in hot climates, where sweating is common, may experience fungal acne more frequently.
What Are The Symptoms Of Fungal Acne?
One of the reasons fungal acne lasts so long is that it looks similar to bacterial acne or acne vulgaris.
Not knowing the difference, people with fungal acne can treat it with regular skin care options. These treatments don't always work and can worsen the infection.
Here's how to tell the difference between bacterial acne and fungal acne:
- Size: The pus-filled spots caused by fungal acne are almost identical. Bacterial acne can cause various-sized pimples and whiteheads.
- Location: Fungal acne often appears on the chest, arms, and back. It can also occur on the face, where bacterial acne is most common.
- Itchy: Fungal acne often causes itching. Bacterial acne is rare.
- Clusters: Fungal acne often appears as clusters of tiny whiteheads. Bacterial acne is less clustered and sparser.
Fungal acne results from yeast overgrowth so you may experience other yeast-related conditions like dandruff and psoriasis. It can help determine if your breakouts are from yeast or another cause.
How Is Fungal Acne Treated?
Fungal acne mistreats because it looks like regular acne. Many people use daily anti-acne treatments against this, but these will not work.
To properly treat your fungal infection, you must restore the balance between the yeast and bacteria on the skin. Several treatment options can help do this.
- Shower More Regularly.
- Wear Loose Clothing.
- Try A Body Wash.
- Use an Over-The-Counter (OTC) Antifungal Treatment.
1. Shower More Regularly
If you exercise regularly or have a job that makes you sweat, try showering and changing right after the gym or work
It can help wash away excess yeast that can begin to grow in the warm, moist environment that develops in sweaty clothes.
2. Wear Loose Clothing
If you frequently wear tight clothing, the friction and reduced airflow can promote yeast growth on the skin.
Choose loose, breathable clothing more regularly to allow your skin to get proper circulation and promote fungal growth and balanced bacteria.
3. Try A Body Wash
Dandruff shampoos made with selenium sulfide or pyrithione zinc can use as a body wash. It is an off-label use of these shampoos, but it can be effective.
Wash your skin with these dandruff shampoos several times a week during breakouts.
Use it about once a week to help maintain a balance of bacteria and yeast on your skin. For best results, leave the shampoo on your skin for several minutes before rinsing.
4. Use an Over-The-Counter (OTC) Antifungal Treatment
Various OTC antifungal creams and ointments, such as medications for athlete's foot and jock itch, are available.
How Is Fungal Acne Diagnosed?
If you believe you have fungal acne symptoms, consider seeing a dermatologist. Dermatologists specialize in treating and diagnosing conditions that affect the skin.
To determine if your symptoms result from fungal acne, the dermatologist will ask you about the symptoms you are experiencing. It will likely include the following:
- How long have you had breakouts?
- What have you used to treat it?
- What symptoms are you experiencing?
In some cases, the examiner may also want to do one of the following:
- They can perform a simple and painless skin scraping to examine the scraping under a microscope. It will look for any yeast responsible for fungal acne.
- They may take a biopsy or skin sample. It is a simple process done in the office. The model will be sent to a laboratory to be tested to confirm the diagnosis of fungal acne.
How Can I Prevent Fungal Acne?
Although fungal acne cannot wholly prevent, these steps can help reduce the chance of a return infection:
For Protecting your fungal acne, you need to follow these amazing home remedies to reduce your acne.
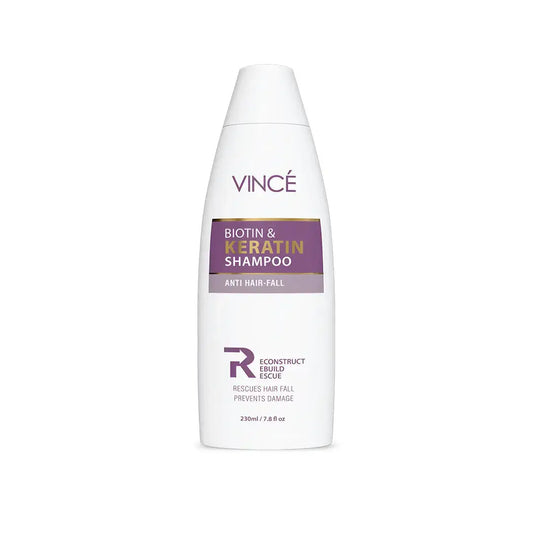
Use Biotin Keratin Shampoo regularly: this regular rinse can help maintain a balance of yeast on your skin. After the breakouts subside, you can reduce the shampoo used as a body washes to at least once a week.
Wear breathable clothing: Breathable clothing allows airflow, reducing the warm, moist environment that encourages fungus growth. If the cloth-changing option helps treat fungal acne, consider wearing the same type of cloth.
Shower after sweating: A quick shower after a workout or a sweaty day at work can help prevent yeast overgrowth problems.
Eat a balanced diet: Fungi, like yeast, thrive on sugary carbohydrates, so balance your diet with fruits, vegetables, and protein to discourage overgrowth.
Conclusion
Fungal acne is a common skin condition when hair follicles become infected with a fungus type called Malassezia yeast. This condition is also called Malassezia folliculitis or Pterosporum folliculitis.
Fungal acne causes clusters of small, itchy, red spots (papules) on your skin. Sometimes, the lumps get a little bigger and turn into whiteheads, small pockets of white or yellow pus (pustules). Despite the name, it is not the same as acne, which causes whiteheads and blackheads.
Common anti-acne treatments will not work for fungal acne. Instead, you need to identify this type of infection correctly so that it can treat appropriately.